What You Need To Know About Insulin Resistance: Understanding its Effects and How to Naturally Reverse It in 7 Simple Steps
Insulin Resistance: Understanding its Effects and How to Naturally Reverse it
Overview
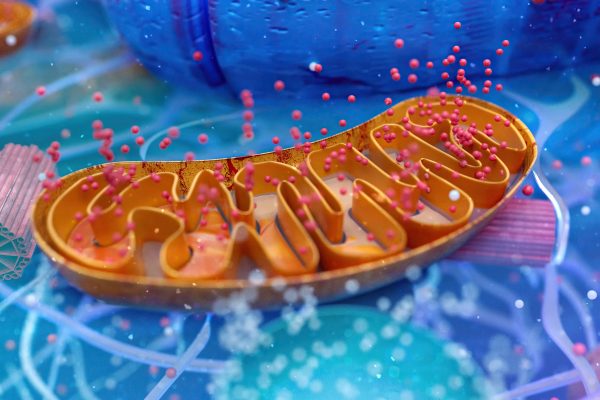
Insulin resistance is a condition in which the body’s cells become less responsive to the hormone insulin. Insulin plays a crucial role in regulating blood sugar levels by facilitating the uptake of glucose from the bloodstream into cells. When cells become resistant to insulin, glucose remains in the bloodstream, leading to high blood sugar levels.
What Causes Insulin Resistance: A Simple Explanation and its Development
In simple terms, insulin resistance is like having a door with a rusty lock. Insulin, the key, tries to unlock the door (your cells) to let glucose (sugar) in, but it
Development of Insulin Resistance
- Genetics: Some people may inherit genes that make them more likely to develop insulin resistance. However, lifestyle factors play a significant role in whether these genes are expressed.
- Unhealthy Diet: A diet high in sugary and processed foods can lead to spikes in blood sugar levels, which over time can contribute to insulin resistance. These foods can also lead to obesity, another risk factor for insulin resistance.
- Lack of Exercise: Physical inactivity can contribute to insulin resistance by making your cells less sensitive to insulin. Exercise helps your cells use glucose for energy, reducing the need for insulin.
- Excess Weight: Being overweight, especially around the abdomen, is strongly linked to insulin resistance. Fat cells, especially visceral fat, release substances that can interfere with insulin’s action.
- Age and Hormones: As you age, your cells may become less responsive to insulin. Hormonal changes, such as those associated with puberty, pregnancy, or menopause, can also affect insulin sensitivity.
- Chronic Inflammation: Inflammation in the body can interfere with insulin signaling, contributing to insulin resistance. This inflammation can be caused by factors such as stress, poor diet, or underlying health conditions.
Insulin resistance develops when your cells become less responsive to insulin, leading to high blood sugar levels. While genetics play a role, lifestyle factors such as diet, exercise, and weight management are key in its development. Understanding these factors can help you make healthier choices to reduce your risk of insulin resistance and related health issues.
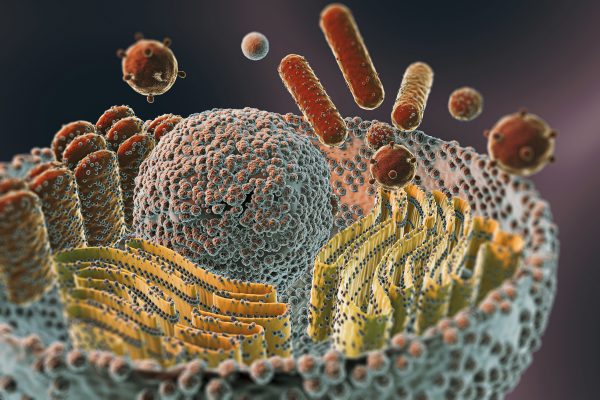
Role of the Pancreas in Insulin Resistance
Insulin resistance is closely linked to the pancreas, as the pancreas plays a central role in the regulation of blood sugar levels and the development of insulin resistance.
- Insulin Production: The pancreas is responsible for producing insulin, a hormone that helps regulate blood sugar levels by facilitating the uptake of glucose from the bloodstream into cells.
- Response to Insulin Resistance: In the early stages of insulin resistance, the pancreas compensates by producing more insulin to overcome the reduced sensitivity of cells to insulin. This increased insulin production helps maintain normal blood sugar levels.
- Progression to Type 2 Diabetes: Over time, however, the pancreas may become unable to produce enough insulin to overcome insulin resistance, leading to a gradual rise in blood sugar levels. This progression can eventually lead to the development of type 2 diabetes.
- Beta-Cell Function: Insulin resistance is often accompanied by a decline in beta-cell function, the cells in the pancreas responsible for producing insulin. This decline in beta-cell function further contributes to the development of type 2 diabetes.
The pancreas plays a critical role in the development and progression of insulin resistance. As insulin resistance develops, the pancreas responds by producing more insulin to maintain normal blood sugar levels. However, over time, the pancreas may become unable to produce enough insulin, leading to the development of type 2 diabetes. Understanding the relationship between insulin resistance and the pancreas is crucial for developing strategies to prevent and manage diabetes.
Hormonal Imbalance and Insulin Resistance
Insulin resistance can have significant effects on hormone levels in both males and females.
Effects on Male Hormones
- Testosterone: Insulin resistance is associated with lower levels of testosterone in men. This can lead to symptoms such as decreased libido, erectile dysfunction, and reduced muscle mass.
- Estrogen: Insulin resistance can also affect estrogen levels in men, leading to an imbalance between testosterone and estrogen. This imbalance can contribute to gynecomastia (enlargement of male breast tissue) and other hormonal issues.
Effects on Female Hormones
- Estrogen and Progesterone: Insulin resistance can disrupt the balance between estrogen and progesterone in women, leading to irregular menstrual cycles, fertility issues, and an increased risk of conditions such as polycystic ovary syndrome (PCOS).
- Testosterone: Women with insulin resistance may experience higher levels of testosterone, which can lead to symptoms such as acne, hirsutism (excessive hair growth), and menstrual irregularities.
Mechanisms of Hormonal Effects
- Insulin and Sex Hormone Binding Globulin (SHBG): Insulin resistance can lead to lower levels of SHBG, a protein that binds to sex hormones such as testosterone and estrogen. This can result in higher levels of free, active hormones in the bloodstream.
- Inflammation: Insulin resistance is associated with chronic inflammation, which can disrupt hormone production and signaling in the body.
- Ovarian Dysfunction: In women, insulin resistance can contribute to ovarian dysfunction, leading to irregular ovulation and imbalances in hormone levels.
Insulin resistance can have profound effects on hormone levels in both men and women. These hormonal imbalances can lead to a variety of symptoms and health issues. Managing insulin resistance through lifestyle changes such as diet, exercise, and stress management is important for maintaining hormonal balance and overall health.
Effects of Insulin Resistance on the Body and Health
- Increased Risk of Type 2 Diabetes: Insulin resistance is a major risk factor for developing type 2 diabetes. When the pancreas can no longer produce enough insulin to overcome the resistance, blood sugar levels rise, resulting in diabetes.
- Cardiovascular Complications: Insulin resistance is associated with an increased risk of heart disease and stroke. High blood sugar levels can damage the blood vessels and lead to atherosclerosis (hardening of the arteries).
- Weight Gain and Obesity: Insulin resistance is often accompanied by weight gain, especially around the abdomen. Excess weight, particularly visceral fat, further contributes to insulin resistance, creating a vicious cycle.
- Hormonal Imbalance: Insulin resistance can disrupt hormonal balance, leading to conditions such as polycystic ovary syndrome (PCOS) in women and low testosterone levels in men.
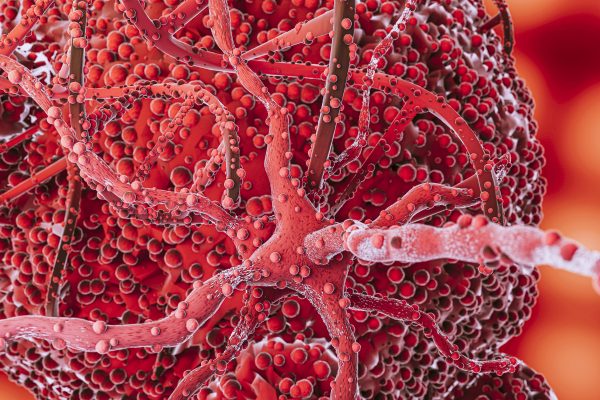
- Increased Inflammation: Insulin resistance is linked to chronic inflammation, which plays a role in the development of various diseases, including cancer and autoimmune disorders.
Diseases Caused by Insulin Resistance
Insulin resistance is associated with an increased risk of several diseases and health conditions:
- Type 2 Diabetes: Insulin resistance is a major risk factor for developing type 2 diabetes. When the pancreas can no longer produce enough insulin to overcome the resistance, blood sugar levels rise, leading to diabetes.
- Cardiovascular Diseases: Insulin resistance is linked to an increased risk of heart disease and stroke. High blood sugar levels can damage the blood vessels and lead to atherosclerosis (hardening of the arteries).
- Obesity: Insulin resistance is often accompanied by weight gain, especially around the abdomen. Excess weight, particularly visceral fat, further contributes to insulin resistance, creating a vicious cycle.
- Hypertension (High Blood Pressure): Insulin resistance is associated with an increased risk of hypertension, which can further increase the risk of heart disease and stroke.
- Non-Alcoholic Fatty Liver Disease (NAFLD): Insulin resistance is a key factor in the development of NAFLD, a condition characterized by excess fat accumulation in the liver.
- Polycystic Ovary Syndrome (PCOS): Insulin resistance is common in women with PCOS and is believed to play a role in the hormonal imbalances characteristic of the condition.
- Certain Cancers: Insulin resistance and the resulting high insulin levels may contribute to the development of certain cancers, including breast, colon, and pancreatic cancer.
- Alzheimer’s Disease: Some studies suggest that insulin resistance and diabetes may increase the risk of developing Alzheimer’s disease and other forms of dementia.
- Chronic Kidney Disease: Insulin resistance is associated with an increased risk of chronic kidney disease, possibly due to its effects on blood sugar control and blood vessel health.
Natural Ways to Reverse Insulin Resistance
- Dietary Changes: A healthy diet is crucial for managing insulin resistance. Focus on whole, unprocessed foods such as fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit sugary foods and refined carbohydrates, which can spike blood sugar levels.
- Regular Exercise: Physical activity can improve insulin sensitivity and help manage weight. Aim for a combination of aerobic exercise (such as walking, jogging, or cycling) and strength training.
- Weight Loss: Losing excess weight, especially around the abdomen, can significantly improve insulin sensitivity. Even modest weight loss can have a positive impact.
- Stress Management: Chronic stress can contribute to insulin resistance. Practice stress-reducing activities such as yoga, meditation, or deep breathing exercises.
- Adequate Sleep: Lack of sleep can disrupt hormone levels and worsen insulin resistance. Aim for 7-9 hours of quality sleep per night.
- Eliminate Alcohol Intake: Excessive alcohol consumption can impair insulin sensitivity. If you choose to drink, understand that it has negative consequences on your health.
- Herbal Supplements: Some herbs, such as berberine, fenugreek, and cinnamon, may help improve insulin sensitivity. However, consult with a healthcare professional before taking any supplements.
Natural Supplements for Insulin Resistance
Natural supplements may help improve insulin sensitivity and potentially reverse insulin resistance. These supplements often work by targeting various mechanisms in the body that influence insulin sensitivity, such as reducing inflammation, improving glucose uptake, and enhancing insulin signaling pathways. However, it’s essential to consult with a healthcare professional before starting any new supplement regimen, as they can interact with medications or have side effects. Here are a few of them:
- Berberine: Berberine is a compound found in several plants, including goldenseal and barberry. Studies have shown that berberine can improve insulin sensitivity, reduce blood sugar levels, and may be as effective as some diabetes medications in managing blood sugar.
- Fenugreek: Fenugreek is an herb commonly used in cooking and traditional medicine. It contains soluble fiber, which can help slow down the absorption of carbohydrates and improve blood sugar control. Fenugreek may also enhance insulin sensitivity.
- Cinnamon: Cinnamon contains compounds that can mimic the effects of insulin and improve insulin sensitivity. Studies suggest that cinnamon supplementation may help lower fasting blood sugar levels and improve insulin resistance.
- Alpha-Lipoic Acid (ALA): ALA is a powerful antioxidant that has been shown to improve insulin sensitivity and reduce symptoms of neuropathy in people with diabetes. ALA may also help reduce inflammation and oxidative stress, which can contribute to insulin resistance.
- Chromium: Chromium is a mineral that plays a role in insulin signaling and glucose metabolism. Some studies suggest that chromium supplementation may improve insulin sensitivity, especially in people with chromium deficiency.
- Magnesium: Magnesium is involved in over 300 enzymatic reactions in the body, including those related to insulin sensitivity and glucose metabolism. Low magnesium levels have been associated with insulin resistance, and supplementation may help improve insulin sensitivity.
How Natural Supplements Help Reverse Insulin Resistance
- Improving Glucose Uptake: Some supplements, such as berberine and cinnamon, can enhance the uptake of glucose by cells, reducing blood sugar levels.
- Enhancing Insulin Signaling: Supplements like ALA and chromium may improve insulin signaling pathways, making cells more responsive to insulin.
- Reducing Inflammation: Chronic inflammation can contribute to insulin resistance. Supplements with anti-inflammatory properties, such as curcumin (from turmeric), may help improve insulin sensitivity.
- Regulating Hormones: Certain supplements, such as fenugreek, may help regulate hormones involved in glucose metabolism, potentially improving insulin sensitivity.
While these natural supplements show promise in improving insulin sensitivity, it’s important to remember that they are not a replacement for a healthy diet and lifestyle. Always consult with a healthcare professional before starting any new supplement regimen, especially if you have diabetes or are taking medications.
Food That Helps Reverse Insulin Resistance
Several foods can help improve insulin sensitivity and potentially reverse insulin resistance when included as part of a balanced diet. Here are some examples:
- Fiber-Rich Foods: Fiber slows down the absorption of sugar into the bloodstream, which can help improve blood sugar control. Include plenty of fruits, vegetables, whole grains, legumes, and nuts in your diet.
- Healthy Fats: Foods rich in healthy fats, such as avocados, olive oil, nuts, and seeds, can help improve insulin sensitivity. These fats are also beneficial for heart health.
- Protein: Including lean protein sources, such as chicken, fish, tofu, and legumes, in your meals can help regulate blood sugar levels and improve insulin sensitivity.
- Low-Glycemic Index Foods: Foods with a low glycemic index (GI) cause a slower and lower rise in blood sugar levels. Examples include whole grains, legumes, non-starchy vegetables, and most fruits.
- Spices and Herbs: Certain spices and herbs, such as cinnamon, turmeric, ginger, and garlic, have been shown to improve insulin sensitivity and reduce inflammation.
- Green Tea: Green tea contains compounds that may improve insulin sensitivity and reduce the risk of developing type 2 diabetes.
- Fatty Fish: Fatty fish like salmon, mackerel, and sardines are rich in omega-3 fatty acids, which have been shown to improve insulin sensitivity.
- Apple Cider Vinegar: Some studies suggest that apple cider vinegar may improve insulin sensitivity and lower blood sugar levels when consumed with meals.
- Probiotic-Rich Foods: Foods containing probiotics, such as yogurt, kefir, and sauerkraut, may help improve insulin sensitivity and reduce inflammation.
Including these foods in your diet, along with regular physical activity and weight management, can help improve insulin sensitivity and potentially reverse insulin resistance. However, it’s important to consult with a healthcare provider or a dietitian before making significant changes to your diet, especially if you have diabetes or other health conditions.
Fasting and Insulin Resistance
Fasting can help reverse insulin resistance through several mechanisms:
- Improved Insulin Sensitivity: Fasting can improve insulin sensitivity, allowing cells to more effectively take up glucose from the bloodstream. This helps lower blood sugar levels and reduce the demand for insulin production.
- Reduced Inflammation: Fasting has been shown to reduce markers of inflammation in the body. Chronic inflammation can contribute to insulin resistance, so reducing inflammation can help improve insulin sensitivity.
- Increased Autophagy: Fasting can stimulate a process called autophagy, where cells remove damaged components and recycle them for energy. This process can help improve cell function and insulin sensitivity.
- Regulation of Hormones: Fasting can affect the levels of various hormones involved in metabolism, including insulin, glucagon, and growth hormone. These hormonal changes can improve insulin sensitivity and help regulate blood sugar levels.
- Weight Loss: Fasting can lead to weight loss, especially fat loss around the abdomen. Excess weight, particularly visceral fat, is strongly associated with insulin resistance, so losing weight can help improve insulin sensitivity.
- Improved Blood Lipids: Fasting can lead to improvements in blood lipid levels, including reductions in triglycerides and LDL cholesterol. This can help reduce the risk of developing insulin resistance and related metabolic disorders.
Fasting can be an effective strategy for reversing insulin resistance by improving insulin sensitivity, reducing inflammation, promoting autophagy, and aiding in weight loss. However, fasting may not be suitable for everyone, especially those with certain medical conditions or eating disorders. It’s important to consult with a healthcare provider before starting any fasting regimen.
After Thoughts
Insulin resistance is a serious condition that can have far-reaching effects on your health. However, with lifestyle changes such as a healthy diet, regular exercise, and stress management, it is possible to improve insulin sensitivity and reduce the risk of developing diabetes and other related health issues. Always consult with a healthcare professional before making any significant changes to your diet or lifestyle.
For natural and healing remedies, products, and supplements to help you live your most optimal healthy life, visit our store here!
Remember: Own Your Health!
If you enjoyed the information presented in this article, Please Share It. Help us reach more people and keep this website going! Thank you!
Note: The information provided in this article is for educational purposes only and should not be considered medical advice. Please consult with a healthcare professional or registered dietitian before making any significant changes to your diet or lifestyle.
References:
- American Diabetes Association. (n.d.). Insulin Resistance and Prediabetes. Retrieved from https://www.diabetes.org/diabetes/insulin-resistance-prediabetes
- Mayo Clinic. (2022). Insulin Resistance. Retrieved from https://www.mayoclinic.org/diseases-conditions/insulin-resistance/symptoms-causes/syc-20355999
- Harvard T.H. Chan School of Public Health. (2020). Diet and Insulin Resistance. Retrieved from https://www.hsph.harvard.edu/nutritionsource/healthy-weight/diet-reviews/diet-and-insulin-resistance/
- Zhang, Y., Li, X., Zou, D., Liu, W., Yang, J., Zhu, N., … & Yang, J. (2008). Treatment of type 2 diabetes and dyslipidemia with the natural plant alkaloid berberine. Journal of Clinical Endocrinology & Metabolism, 93(7), 2559-2565.
- Neelakantan, N., Narayanan, M., de Souza, R. J., van Dam, R. M., & Nanda, N. C. (2014). Effect of fenugreek (Trigonella foenum-graecum L.) intake on glycemia: a meta-analysis of clinical trials. Nutrition journal, 13(1), 1-10.
- Qin, B., Panickar, K. S., & Anderson, R. A. (2010). Cinnamon: potential role in the prevention of insulin resistance, metabolic syndrome, and type 2 diabetes. Journal of Diabetes Science and Technology, 4(3), 685-693.
- Midaoui, A. E., Elimadi, A., & Wu, L. (2003). HPLC determination of α-lipoic acid in tissues and subcellular compartments of rat liver. Journal of pharmaceutical and biomedical analysis, 31(2), 293-301.
- Cefalu, W. T., Hu, F. B., & Role of chromium in human health and in diabetes. (2004). Diabetes Care, 27(11), 2741-2751.
- Barbagallo, M., Dominguez, L. J., & Magnesium and type 2 diabetes. (2015). World journal of diabetes, 6(10), 1152-1157.
- Mauvais-Jarvis, F. (2015). Sex differences in metabolic homeostasis, diabetes, and obesity. Biology of Sex Differences, 6(1), 14. https://doi.org/10.1186/s13293-015-0033-y
- Dandona, P., Dhindsa, S., Chaudhuri, A., Bhatia, V., Topiwala, S., Mohanty, P., & Ghanim, H. (2009). Hypogonadotrophic hypogonadism in type 2 diabetes, obesity and the metabolic syndrome. Current Molecular Medicine, 9(9), 1105–1117. https://doi.org/10.2174/156652409789838767
- Patterson, R. E., & Sears, D. D. (2017). Metabolic Effects of Intermittent Fasting. Annual Review of Nutrition, 37, 371–393. https://doi.org/10.1146/annurev-nutr-071816-064634
- Antoni, R., Johnston, K. L., & Collins, A. L. (2018). Intermittent v. continuous energy restriction: differential effects on postprandial glucose and lipid metabolism following matched weight loss in overweight/obese participants. British Journal of Nutrition, 119(5), 507–516. https://doi.org/10.1017/S0007114517003890























1 Comment
[…] cancer, and cardiovascular disorders. By enhancing autophagy, we can potentially reduce the risk of these diseases and promote healthier […]