What You Need to Know About Fatty Liver: An In-depth Analysis of its Causes, Remedies, and 5 Simple Tips for Prevention
Fatty Liver: An In-depth Analysis of its Causes and Remedies
Overview
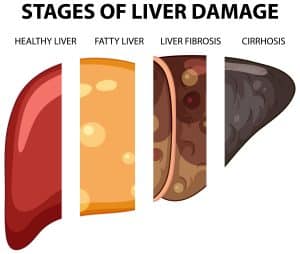
In this article, you’ll discover not just the causes and symptoms of fatty liver disease, but also how lifestyle choices contribute to its development. You’ll learn about effective treatment and management options that might pose the question: “Can fatty liver be reversed?” Additionally, the role of diet in managing and potentially reversing fatty liver disease will be explored, alongside measures to prevent its onset. Even for individuals concerned about cirrhosis, a severe liver condition often linked with alcoholic liver disease, this analysis will provide valuable insights.
Understanding Fatty Liver Disease
Understanding the Types of Fatty Liver Disease:
- Nonalcoholic Fatty Liver Disease (NAFLD):
-
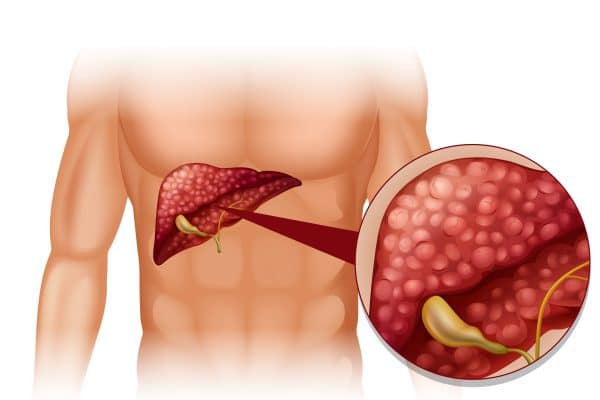
- Simple Fatty Liver (NAFL): Characterized by the accumulation of fat in the liver without hepatocellular injury. It is generally considered less severe and has a lower risk of progressing to more serious liver conditions.
-
- Nonalcoholic Steatohepatitis (NASH): A more serious form of NAFLD, involving not only fat accumulation but also inflammation and damage to liver cells. This can progress to fibrosis, cirrhosis, and even liver cancer if not addressed.
- Alcoholic Liver Disease (ALD):
-
- Occurs as a result of excessive alcohol consumption. It starts as fatty liver, an early and reversible stage, but can progress to more serious conditions like alcoholic hepatitis and cirrhosis if alcohol consumption continues.
Risk Factors and Diagnosis:
- Risk Factors:
-
- NAFLD: Strongly associated with metabolic syndrome, including conditions like obesity, type II diabetes, and hypertriglyceridemia. A family history of liver disease can also increase the risk.
-
- ALD: Risk factors include genetics, minimum amounts of alcohol intake, hepatitis C virus (HCV) antibody, iron overload, and obesity.
- Diagnosis:
-
- Involves a combination of blood tests, imaging procedures, and sometimes a liver biopsy. Blood tests can include liver function tests, fasting blood sugar, and lipid profiles. Imaging tests like abdominal ultrasound and MRI help in assessing liver fat and damage.
Prevalence and Public Health Impact:
- Prevalence:
-
- NAFLD affects approximately 25% of the global population and is the most common liver disorder in the Western world. It affects 1 in 3 adults in the US, highlighting its significant public health impact.
- Public Health Issue:
-
- NAFLD is closely linked to obesity and metabolic disorders, making it a significant public health concern. The condition’s prevalence and its association with serious health risks underscore the importance of awareness and early intervention.
Symptoms and Diagnosis
Identifying the symptoms of fatty liver disease (FLD) is crucial, as they can range from non-existent to severe, depending on the stage and type of the disease. Recognizing these symptoms early can significantly impact the management and potential reversal of the condition.
- Symptoms of Nonalcoholic Fatty Liver Disease (NAFLD) and Alcoholic Liver Disease (ALD):
- General symptoms include fatigue and discomfort or pain in the upper right abdomen.
-
- Advanced stages, such as Nonalcoholic Steatohepatitis (NASH) and cirrhosis, may exhibit more specific symptoms like itchy skin, abdominal swelling, shortness of breath, swelling of the legs, spider-like blood vessels beneath the skin’s surface, enlarged spleen, red palms, and jaundice (yellowing of the skin and eyes).
- Diagnosis Procedures:
-
- The diagnosis of FLD involves a comprehensive approach including a health history review and physical examination, alongside various tests.
- Blood Tests: To check liver enzyme levels and other markers indicative of liver health.
- Imaging Tests: Such as ultrasound, CT scans, or MRI, to visualize fat accumulation and liver damage.
- Liver Biopsy: Although not always necessary due to advancements in non-invasive tests, it remains the gold standard for diagnosing and staging FLD.
- Non-invasive markers and tests, like the NAFLD Fibrosis Score, ELF test, and transient elastography, are increasingly used to identify patients with advanced disease stages without the need for a biopsy.
- The diagnosis of FLD involves a comprehensive approach including a health history review and physical examination, alongside various tests.
- Challenges in Diagnosis:
-
- Despite the availability of diagnostic tools, many patients with NAFLD remain undiagnosed. A significant challenge is the reliance on abnormal liver enzyme levels to identify NAFLD, which can lead to overlooking patients with significant liver disease.
-
- NAFLD is often discovered incidentally during tests for other health issues, underscoring the importance of recognizing at-risk individuals and the need for routine screening in certain populations.
This section highlights the importance of being aware of the potential symptoms associated with fatty liver disease and the comprehensive approach required for accurate diagnosis. Early detection and diagnosis are key to managing the disease effectively and preventing its progression.
Lifestyle Contributions to Fatty Liver
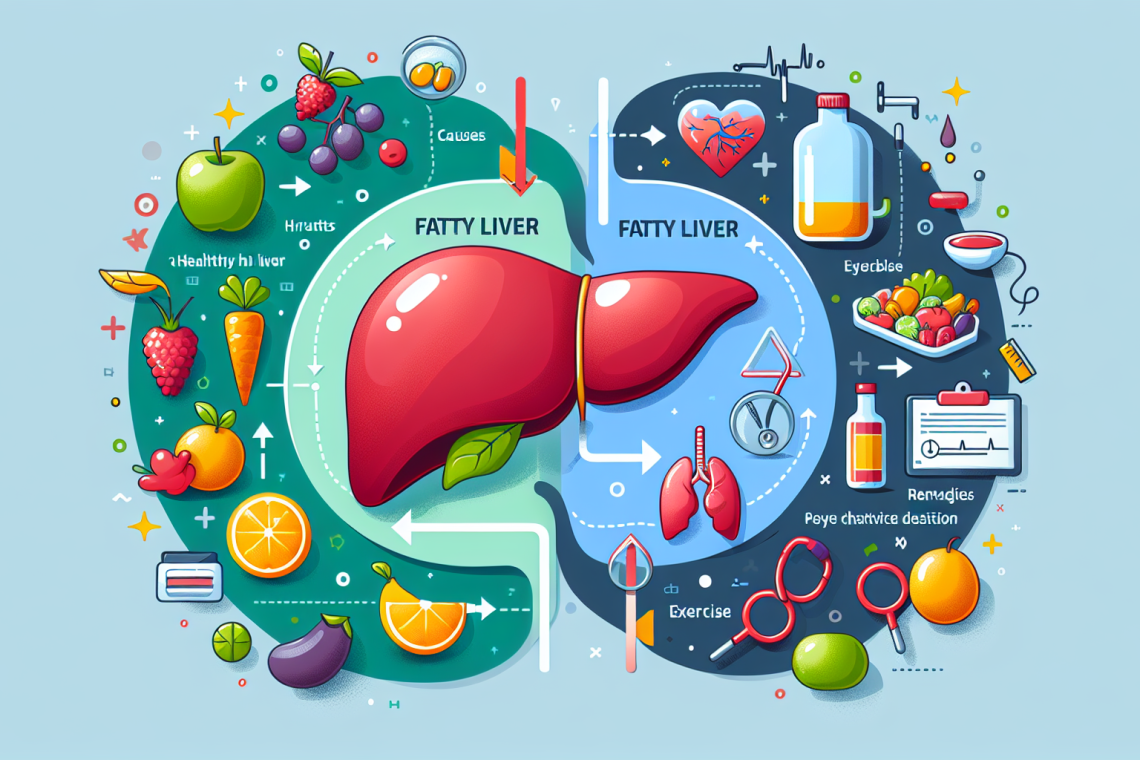
Lifestyle choices play a pivotal role in the development and management of fatty liver disease. By understanding and adjusting these factors, individuals can significantly impact their liver health.
-
- Limit Alcohol Consumption: To prevent the onset and progression of fatty liver disease, it’s crucial to moderate alcohol intake.
-
- Control Calorie Intake: Avoiding excessive calories is essential as it leads to fat buildup in the liver. This is particularly important in the context of the Western diet, which is rich in processed and high-fat foods.
-
- Reduce Sugar and Processed Foods and Fats: Monitoring sugar intake, especially from sweetened drinks and desserts, helps prevent fat accumulation. Also, processed fats such as vegetable oils (Canola oil, Safflower oil, Corn Oils, Peanut Oil, etc.) should be avoided. Ultra-processed foods and fats and sugar-sweetened beverages are significant contributors to NAFLD.
- Physical Activity:
-
- Engage in Regular Exercise: Starting to exercise can independently lead to NAFLD remission. Both aerobic activity and resistance training have shown similar effects in reducing hepatic fat.
-
- Intensity and Frequency: While universal recommendations for the optimal intensity and dose of physical activity have not been established, even minimal physical activity below the recommended threshold can beneficially impact NAFLD.
-
- Weight Loss: Steatosis, or fatty liver, may be reversible with weight loss. Larger weight loss is associated with a higher frequency of NAFLD remission, highlighting the importance of sustained lifestyle changes.
-
- Challenges in Sustained Changes: Achieving and maintaining weight loss is challenging, and lifestyle changes alone may not be successful for every individual. However, lifestyle modifications remain the treatment of choice for NAFLD due to the lack of approved pharmacologic agents.
Understanding these lifestyle factors is critical in managing and potentially reversing fatty liver disease. By focusing on dietary habits, engaging in regular physical activity, and managing weight, individuals can significantly reduce their risk and improve their liver health.
Treatment and Management Options
When addressing the treatment and management options for fatty liver disease, a multifaceted approach is recommended. This includes lifestyle changes, medical interventions, and in some cases, surgical options. Below is a detailed overview:
Lifestyle Modifications
- Weight Management: Achieving a weight loss of 7-10% of baseline weight can significantly improve liver fat, inflammation, and fibrosis. Even a modest weight loss of 5% can lower liver fat.
- Diet and Exercise: A balanced diet alongside regular physical activity is crucial. Treatment often begins with dietary adjustments, portion control, and engaging in exercise routines. Specific nutritional interventions such as food selection and time-restricted eating (Intermittent Fasting) may also be beneficial. Doing a liver cleanse at least twice a year with Natural Fresh Organic juices and supplements is also very beneficial.
- Alcohol and Medications: For individuals with alcoholic fatty liver disease, discontinuing alcohol consumption is essential. Additionally, protecting liver health involves careful use of natural foods, supplements, and medications only if necessary.
Medical Management
- Diabetes and Cholesterol Control: Managing underlying conditions such as diabetes and keeping cholesterol and triglycerides in check through a healthy diet, exercise, and medication if necessary, are vital steps.
- Drug Therapy: While lifestyle modifications are the cornerstone of treatment, Vitamin E and pioglitazone have emerged as drug options for biopsy-proven NASH, although their long-term effectiveness and safety require careful consideration. New pharmacotherapies for NASH and fibrosis are also under investigation.
Surgical Interventions
- Bariatric Surgery: In severe cases, particularly for obese individuals who have not succeeded in losing weight through lifestyle changes or medication, bariatric surgery may be considered. This should be the very last option.
It’s imperative to note that the prognosis varies depending on the type of fatty liver disease and the presence of other conditions. For instance, simple alcoholic steatosis has a favorable outcome once alcohol consumption stops. However, ALD generally has a worse prognosis in patients with cirrhosis compared to those with chronic hepatitis C infection or NAFLD-related cirrhosis. Regular screening and liver health maintenance are crucial aspects of managing fatty liver disease, emphasizing the importance of early detection and intervention.
The Role of Diet in Managing Fatty Liver
Your diet is everything, and you mut let your food be your medicine and your medicine be your food. In managing fatty liver disease, dietary choices play a crucial role. The Mediterranean diet, characterized by its rich inclusion of fruits, vegetables, nuts, whole grains, and lean sources of protein such as white meat and fish, comes highly recommended for those looking to manage or reverse fatty liver disease. This diet’s effectiveness is attributed to its balanced composition of healthy fats, antioxidants, and complex carbohydrates.
Recommended Foods:
- Healthy Fats: Incorporate foods high in Omega-3 fatty acids and monounsaturated fats, such as fish, seafood, avocados, and olive oil. These fats improve the body’s insulin sensitivity, reducing fat buildup in the liver.
- Whole Grains and Legumes: Opt for whole grains and legumes, which are integral to the Mediterranean diet, to ensure a rich intake of complex carbohydrates.
- Antioxidant-Rich Foods: Include coffee, green tea, raw garlic, and a variety of fruits and vegetables to benefit from antioxidants that protect cells from damage and help reduce fat buildup in the liver.
Foods to Limit or Avoid:
- Seed Oils: Avoid foods high in seed oils or vegetable oils. These contribute to increased inflammation throughout your body and fatty deposits in the liver.
- Added Sugars and Processed Foods: Minimize intake of sugary beverages, desserts, and ultra-processed foods to prevent fat accumulation.
In addition to dietary modifications, integrating regular physical activity, specifically aerobic and resistance training, can significantly impact liver health by reducing liver fat and inflammation. Moreover, dietary supplements such as goji berry, resveratrol, selenium, milk thistle, and berberine are being studied for their potential benefits to liver health, although their effectiveness in the treatment of fatty liver disease requires further investigation.
By adhering to these dietary guidelines and incorporating regular exercise, individuals can manage and potentially reverse fatty liver disease, improving their overall liver health and reducing the risk of progression to more severe liver conditions.
Preventing Fatty Liver Disease
Preventing fatty liver disease (FLD) involves a combination of lifestyle choices that support overall liver health. By adhering to the following practices, you can significantly reduce your risk of developing this condition:
- Healthy Weight Maintenance:
-
- Engage in regular physical activities that you enjoy, such as walking, swimming, or cycling, to maintain a healthy weight.
-
- Follow a balanced diet rich in fruits, vegetables, lean proteins, and avoid vegetable or seed oils to support weight management.
- Metabolic Risk Factor Management:
-
- Monitor and manage conditions like obesity, type 2 diabetes, and high blood pressure through regular check-ups and following your healthcare provider’s advice.
-
- If you have been diagnosed with metabolic syndrome, adherence to prescribed medications and lifestyle adjustments are crucial for managing the condition.
- Dietary Patterns:
-
- Opt for the Mediterranean diet, which emphasizes the consumption of healthy fats, and a high intake of fruits and vegetables, as it’s shown to be effective in preventing FLD.
-
- Limit the intake of simple sugars and processed foods to minimize the risk of fat accumulation in the liver.
- You can also consider intermittent fasting as an effective means to prevent and reduce fatty liver.
- Alcohol and Portion Control:
-
- Minimize alcohol consumption as it can directly contribute to the development of fatty liver disease.
-
- Practice portion control to avoid excessive calorie intake, which can lead to weight gain and increased liver fat.
- Regular Exercise:
-
- Incorporate both aerobic and resistance training into your routine to improve liver health and reduce fat buildup.
-
- Aim for at least 150 minutes of moderate-intensity exercise per week, as recommended by health guidelines, to maintain a healthy liver.
By integrating these preventive measures into your daily routine, you can effectively reduce your risk of developing fatty liver disease. It’s important to remember that consistency in maintaining a healthy lifestyle is key to preventing not only FLD but also a wide range of other health conditions.
Final Thoughts
Through this comprehensive analysis, we have explored the multifaceted nature of fatty liver disease, delving into its causes, symptoms, and the significant impact of lifestyle choices on its management and potential reversal. The discussion underscored the critical role of dietary habits, physical activity, and weight management in combating this condition. Importantly, we highlighted the effectiveness of the Mediterranean diet and regular exercise as foundational elements in improving liver health and mitigating the risk of progression to more severe liver conditions.
As we conclude, it’s imperative to recognize the power of informed and proactive lifestyle modifications in preventing and managing fatty liver disease. Emphasizing early detection and intervention, along with a commitment to dietary and lifestyle changes, can significantly enhance the prognosis for individuals facing this condition. Moreover, the continued exploration of treatment options underscores the evolving landscape of fatty liver disease management, offering hope and direction for those affected. By adhering to these principles, individuals can substantially improve their liver health, quality of life, and potentially reverse the course of this increasingly prevalent disease.
Start incorporating liver-friendly foods and supplements into your diet today and experience the benefits of a revitalized liver and optimal health.
For natural and healing remedies, products, and supplements to help you live your most optimal healthy life, visit our store here!
Remember: Own Your Health!
If you enjoyed the information presented in this article, Please Share It. Help us reach more people and keep this website going! Thank you!
Note: The information provided in this article is for educational purposes only and should not be considered medical advice. Please consult with a healthcare professional or registered dietitian before making any significant changes to your diet or lifestyle.
FAQs
- How can one quickly recover from fatty liver disease?
To expedite recovery from fatty liver, one can implement several treatments and lifestyle adjustments such as losing weight, taking medications to lower cholesterol or triglycerides, managing blood pressure, controlling diabetes, limiting over-the-counter drugs, abstaining from alcohol, and consulting a liver specialist. - What primarily leads to the development of fatty liver?
Fatty liver typically occurs when the liver is unable to metabolize and break down fats effectively, leading to an excessive accumulation of fat. This condition is commonly associated with other health issues like obesity, diabetes, high triglycerides, and can also be caused by alcohol abuse, rapid weight loss, and malnutrition. - What is the expected lifespan of an individual diagnosed with fatty liver disease?
For individuals with non-alcoholic fatty liver disease (NAFLD), life expectancy may be reduced by approximately 4.2 years for women and 4.4 years for men. - What are the most effective methods for treating fatty liver disease?
Effective treatment for fatty liver disease involves adhering to a healthy diet with limited sugar, achieving and maintaining a healthy weight, engaging in regular physical activity, managing blood sugar levels, treating high cholesterol if present, avoiding medications that can harm the liver, drinking little to no alcohol, and quitting smoking if applicable.
References
[1] – https://medlineplus.gov/fattyliverdisease.html
[2] – https://www.ncbi.nlm.nih.gov/books/NBK441992/
[3] – https://emedicine.medscape.com/article/175472-overview
[4] – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6334080/
[5] – https://fg.bmj.com/content/5/3/211
[6] – https://www.webmd.com/hepatitis/fatty-liver-disease
[7] – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4177476/
[8] – https://www.healthdirect.gov.au/fatty-liver
[9] – https://wexnermedical.osu.edu/blog/fatty-liver-disease
[10] – https://www.mayoclinic.org/diseases-conditions/nonalcoholic-fatty-liver-disease/diagnosis-treatment/drc-20354573
[11] – https://jamanetwork.com/journals/jama/fullarticle/2810964
[12] – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7766941/
[13] – https://www.bmj.com/content/383/bmj-2023-075179
[14] – https://www.mayoclinic.org/diseases-conditions/nonalcoholic-fatty-liver-disease/symptoms-causes/syc-20354567
[15] – https://www.hopkinsmedicine.org/health/conditions-and-diseases/nonalcoholic-fatty-liver-disease
[16] – https://my.clevelandclinic.org/health/diseases/15831-fatty-liver-disease
[17] – https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/liver-fatty-liver-disease
[18] – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7005657/
[19] – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5768549/
[20] – https://bmcgastroenterol.biomedcentral.com/articles/10.1186/s12876-020-01270-7
[21] – https://www.nature.com/articles/s41598-019-57369-9
[22] – https://onlinelibrary.wiley.com/doi/full/10.1111/liv.14360
[23] – https://www.health.harvard.edu/blog/fatty-liver-disease-what-it-is-and-what-to-do-about-it-2019011015746
[24] – https://www.uchicagomedicine.org/forefront/gastrointestinal-articles/fatty-liver-disease-diet
[25] – https://www.jandonline.org/article/S0002-8223(11)01703-2/fulltext





















0 Comment